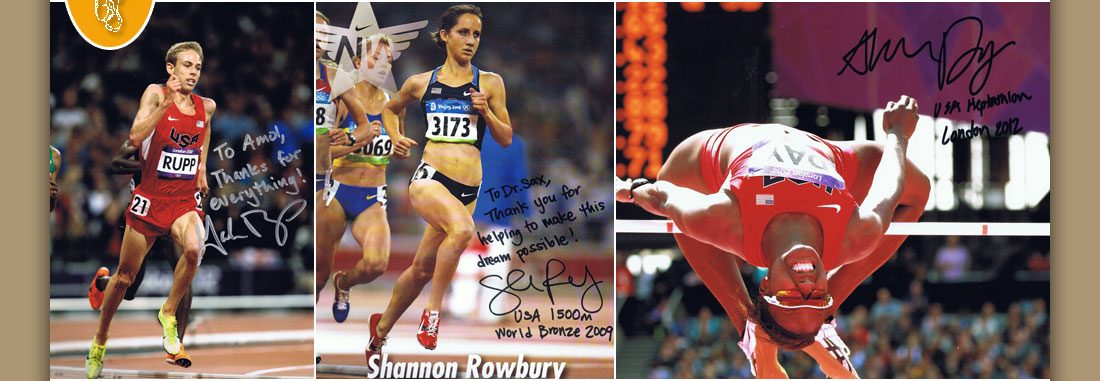

Dr. Amol Saxena, DPM
Palo Alto Foundation
Medical Group
Dept. of Sports Medicine
3rd Floor, Clark Building
795 El Camino Real
Palo Alto, CA 94301
Office: 650-853-2943
Fax: 650-853-6094
E-Mail
Map | Directions

| Articles |
The Ludloff Osteotomy: A Critical Analysis. Journal of Foot and Ankle Surgery, Vol 2, 1997.
Amol Saxena, D.P.M., F.A.C. F.A.S.*
Derek McCammon, D.P.M.
* Address Correspondence to:
Department of Sports Medicine,
Palo Alto Medical Foundation
795 El Camino Real |
Palo Alto, CA 94301 |
First-year Resident, California College of Podiatric Medicine
ABSTRACT
Fourteen Ludloff (oblique shaft) osteotomies were performed to reduce the first intermetatarsal angle on 12 female patients, average age 47 years. Average reduction of the first intermetatarsal angle was 6.5 degrees, (postoperative average 9.4 degrees). Average hallux abductus angle reduction was 16.7 degrees, (postoperative average 13.4 degrees). These reductions were statistically significant (P .05). Average first metatarsal shortening was 1.4 mm. No transfer lesions nor lesser metatarsal stress fractures were noted. One patient (a 30+ pack/year smoker) sustained a delayed union. The average American Orthopedic Foot and Ankle Rating Score was 92.3 out of 100. Average follow up was 48 months. This procedure is a viable alternative to closing base wedge osteotomies.
Key Words: Shaft osteotomy; first metatarsal osteotomy; closing base wedge osteotomy; first intermetatarsal angle.
INTRODUCTION
Numerous procedures have been described in the literature to reduce the metatarsus primus adductus component of moderate hallux abductovalgus. Moderate to severe hallux abductovalgus can be defined as an intermetatarsal angle of 11 - 15 degrees for an adducted foot type, and 13 - 17 degrees in the rectus foot type (1). The closing abductory base wedge osteotomy is often used in place of first metatarsal shaft procedures due to the fear of poor bone healing in diaphyseal bone (2,3). Volger states in his article that "the absolute stability of the postoperative system" compensates for any loss of vasculature during dissection and that most shaft-type osteotomies will heal with primary bone healing (4). The opening abductory base wedge osteotomy, the crescentic osteotomy of the base of the first metatarsal the transpositional/rotational base osteotomy, the wedge shelf osteotomy, as well as the first metatarsal-cuneiform arthrodesis procedures are also viable options to reduce this deformity (4,5).
Since its first description in 1901 by Loison, the transverse closing abductory base wedge osteotomy has received many modifications and is well know for its potential postoperative complications (6). There have been abundant studies that document complications following closing base wedge osteotomies. Schuberth et. al. found that the first metatarsal was elevated an average of 6.679 degrees in the sagittal plane in 93.7% of their cases (7). Zlotoff found that the first metatarsal was shortened an average of 2.6 mm. This shortening alters the weight-bearing pattern of the forefoot causing more stress on the lesser metatarsals during gait (8).
Intraoperatively there is one complication worth noting with the closing base wedge procedure: fracture of the medial cortical hinge. This fracture removes one point of fixation and can lead to dorsiflexion and/or shortening of the first metatarsal, as well as loss of the desired correction. In addition, weight bearing prior to six weeks is also associated with first metatarsal elevation and delayed union (4, 7, 12).
The oblique base wedge osteotomy is a popular modification of the transverse abductory base wedge osteotomy that allows multiplanar correction as well as easy application of AO/ASIF principle for rigid internal fixation. A limited number of first metatarsal shaft-type (diaphyseal) procedures have been described. They include the Scarf (9, 10), offset-V (11,12), Mau (13), and the Ludloff (14) osteotomies. Shaft-type osteotomies are useful to reduce moderate intermetatarsal angles and use rigid internal fixation (4).
The purpose of this paper is to describe the Ludloff (14) osteotomy and to evaluate its effectiveness at reducing a moderate increase in the first intermetatarsal angle of hallux abducto valgus. The Ludloff osteotomy was first described in 1918 and is a through-and-through osteotomy in the transverse plane extending dorsal-proximal to plantar-distal when viewed in the sagittal plane. This osteotomy configuration allows for intermetatarsal angle reduction, lengthening, and plantar displacement. This configuration is not intrinsically stable, therefore fixation is necessary.
SURGICAL PROCEDURE
A dorsomedial skin incision is made extending proximally from the first metatarsal phalangeal joint to the base of the first metatarsal. The capsulotomy is extended proximally through the periosteum of the first metatarsal. The medial aspect of the first metatarsal's periosteum is scored for performance of the oblique shaft osteotomy. The osteotomy extends approximately 1.5 cm from distal to the base of the first metatarsal (dorsal-proximal to plantar-distal), ending proximal to the sesamoid apparatus (Figure 1). The osteotomy should be "biased" dorsal- medial to plantar-lateral in the frontal plane such that when the capital fragment is transposed laterally to reduce the intermetatarsal angle, the metatarsal head will translocate plantarly. More bone can be resected plantarly to allow greater plantar flexion in cases with first metatarsal elevatus. Temporary fixation is accomplished with the guidewires for cannulated screws, or Kirschner wires, and a bone clamp (Figure 2). A bone clamp alone may be used, but this maneuver may to cause loss of correction. Two 2.7 or 3.5 mm cortical screws are used to fixate the osteotomy, generally 14-20 mm in length. (Figures 3). The remaining medial ledge is remodeled (Figure 4). Closure is performed in a typical fashion.
Postoperatively, patients are maintained non-weight bearing in a below-knee splint, cast and/or boot for a total of three weeks. The patients utilize a boot or surgical shoe for an additional two to three weeks and then are allowed to progress to athletic shoes. Athletic activities such as running are allowed at 8 to 10 weeks, and jumping activity such as aerobics/dance are allowed at 10 to 12 weeks. Stationary biking is allowed in the below-knee cast four to seven days postoperatively and swimming is allowed four (metatarsal osteotomy alone) to six weeks postoperatively (when in conjunction with phalangeal osteotomy) The reader is referred to Figures 5 and 6 to review pre- and post-operative x-rays. Low-heel dress shoes are typically able to be worn at 12 weeks when a phalangeal osteotomy (i.e., Akin) is performed. Active range of motion exercises of the first metatarsal phalangeal joint are started at three weeks following surgery. Physical therapy can be instituted at six weeks following surgery; generally, three times a week for two to four weeks. This consists of modalities such as ultrasound, contrast baths and electrical stimulation. Active strengthening exercises along with proprioceptive exercises are also utilized.
MATERIALS AND METHODS
Fourteen patients undergoing osteotomies in conjunction with other procedures from April 1991 to December 1994 by the senior author were evaluated. Pre- and post-operative measurements of first intermetatarsal and hallux abductus angles along with the metatarsal protrusion distance and tibial sesamoid position were evaluated. The measurements were performed on weight-bearing views. The six week postoperative or latest weight-bearing views were also evaluated for the same parameters. Any complications such as symptomatic screws, transfer lesions, delayed unions, etc. were noted. The American Orthopedic Foot and Ankle Society Hallux Rating Scale was utilized to evaluate the results (15).
RESULTS
Fourteen procedures performed on females, median age 47 years were evaluated. Average follow-up was 48 months. The average preoperative intermetatarsal and hallux abductus angles were 15.9 degrees and 30.1 degrees, respectively. Average metatarsal protrusion distance and tibial sesamoid position were -2.7 mm and 5.6, respectively. Postoperative results yielded an average intermetatarsal angle of 9.4 degrees (or a reduction of 6.5 degrees). This was statistically significant (P .05)) using the t-test. Similarly, for hallux abductus angle, postoperatively yielded an average of 13.4 degrees for a reduction of 16.7 degrees. This was also significant (P .05). (Patients undergoing Ludloff procedures alone had an average post-operative hallux abductus angle of 15.4 degrees; for those who also had the Akin procedure the average was 11.3 degrees.) This was statistically significant (P .025). Post-operatively, average shortening of the first metatarsal was 1.4 mm; tibial sesamoid position was 2.9. The average American Orthopedic Foot and Ankle Society Rating Score was 92.3 out of 100.
One patient suffered a delayed union which resolved with the use of an EBI bone stimulator. Another patient necessitated removal of fixation four years later. A third patient complained of second metatarsal phalangeal joint pain plantarly, although no lesion developed.
One patient had a hypermobile first ray and ligamentous laxity. Subsequent to her procedure, she was diagnosed with breast cancer and connective tissue disorders. She developed reoccurrence of the hallux abductus valgus deformity which was mildly symptomatic. The reader is referred to Tables 1 and 2 for the specific data for each patient.
DISCUSSION
Any surgical procedure has its own inherent complications. Patient lifestyle and health status influences the outcome. The one patient that sustained a delayed union was a 30+ pack-year smoker and delayed/nonunion in smokers has been cited by others in foot surgery (16, 17). The one reoccurrence was with the patient with the connective tissue disorder. Perhaps an implant (such as what is performed for rheumatoid patients) and/or first metatarsal cuneiform arthrodesis may have afforded better long-term results for her.
Studies have reported the closing base wedge osteotomy to cause significant shortening of the first metatarsal. Zlotoff found an average of 2.6 mm of shortening with the closing base wedge osteotomy. The procedure described in this paper caused 1.4 mm of shortening - almost 50 percent less (8). This may be significant enough to prevent metatarsalgia that can be seen with the closing base wedge osteotomy. The Ludloff osteotomy allows earlier weight bearing (three weeks vs. six weeks) (4, 7, 12, 18). It also allows for rigid internal fixation. Loss of correction may be due to the osteotomy's tendency to move when temporarily fixating with only a bone clamp. Therefore, provisional fixation with pins/wires and a clamp is very important.
The Ludloff osteotomy for the first metatarsal may be plantarflexed as well as it may be lengthened. This may be helpful in avoiding transfer lesions. (Though first metatarsal elevation was not specifically measured, it can be assessed clinically by the lack, or presence, of lesser metatarsal pathology.) As for lesser metatarsal symptoms, only
1 patient out of 12 suffered sub-second metatarsal phalangeal joint pain, but she did not develop a transfer lesion nor did any other patient.
Seven of these patients did have this procedure in conjunction with an Akin osteotomy. In their paper Cisar et. al. performed the Ludloff/Akin procedure as their prime procedure for hallux abductus valgus deformity. If there is significant arthrosis in the first metatarsal phalangeal joint, they performed a Ludloff/Keller procedure. They performed 72 of these procedures with 6 months to 2½ years follow up and reported no complications. They used A-O screw fixation and maintained their patients non-weight bearing for 12 days; following this, they placed them in a surgical shoe for an additional 4 weeks. This is one of the most popular procedures performed in Germany for hallux abductovalgus deformity (19). Another German paper cites the disadvantage of the Ludloff osteotomy to be delayed healing due to its diaphyseal location, but does not mention the mode of fixation (20).
The senior author has performed this procedure on four additional patients (two males and two females), with less than one year follow-up. The pre-operative intermetatarsal and hallux abductus angles were 17.5 degrees and 34.5 degrees respectively. Post-operative results revealed an average intermetatarsal and hallux abductus angles of 9.25 degrees and 13.75 degrees respectively. Similar long term results as found in this study are anticipated for these four patients.
This paper utilizes the American Foot and Ankle Orthopedic Society's Rating System to evaluate results. The authors encourage the readership to review Kitaoka et. al.'s manuscript and evaluate their rating scale (15). There are several weaknesses of the scale, such as not including factors like toe purchase, delayed healing, and the need for symptomatic hardware removal. Perhaps the American College of Foot and Ankle Surgeons will develop a rating scale of their own. In the interim, a commonly recognized and accepted rating system should be used to aid in objective evaluations.
CONCLUSION
The Ludloff osteotomy is a viable alternative to other first intermetatarsal angle reducing osteotomies such as the base wedge osteotomy. It shortens the first metatarsal less than the closing base wedge osteotomy and allows for plantar flexion. Reduction of first intermetatarsal and hallux abductus angles are at least as comparable to other procedures. The non-weight-bearing phase post-operatively is only three weeks as compared to other procedures requiring six weeks or more. Further use and study of this procedure is warranted.
REFERENCES
1. Palladino, S.J. Preoperative evaluation of the bunion patient, In Textbook of Bunion Surgery, 2nd ed., Ch. 1 pp. 1-87, edited by J. Gerbert, Futura Publishing, Mount Kisco, N.Y., 1991.
2. Rhinelander, F.W., Wilson, J.W., Blood supply to developing, mature, and healing bone, in Clinical Orthopaedics, Ch. 2, pp. 81-158, W.B. Saunders Company, Philadelphia, PA 1982.
3. Jaworek, T.E., The intrinsic vascular supply to the first metatarsal. J. Am. Podiatric Med. Assoc. 63:555-562, 1973.
4. Volger, H.W. Shaft Osteotomies in Hallux Valgus, In Clinics in Podiatric Medicine and Surgery, 6:47-69, edited by M. C. Burns, W. B. Saunders Company, Philadelphia, PA, 1989.
5. Martin, D.E., Blitch, E.L., Alternatives to the closing base wedge osteotomy, In Clinics of Podiatric Medicine and Surgery, 13:515-531, 1996.
6. Loison, M, Note sur le traitment chirugical du hallux valgus d'apres l'etude radiographique de la deformation. Bill. Mem. Soc. Chir. Paris 27:528-531, 1901.
7. Schuberth, J. M., Reilly, C. H., Gudas, C. J., The closing wedge osteotomy. A critical analysis of first metatarsal elevation. J. Am. Podiatric Med. Assoc. 74:13-24, 1984.
8. Zlotoff, H. Shortening of the first metatarsal following osteotomy, and its clinical significance. J. Am. Podiatric Med. Assoc. 67:412-425, 1977.
9. Meyer, M., Eine neve modifikation der hallux valgus operation. Zbl Chir 53:3215-3268, 1926.
10. Zygmunt, K., Gudas, C., Laros, G., Z-bunionectomy with internal screw fixation. J. Am. Podiatric Med. Assoc., 79:322-329, 1989.
11. Volger, H.W., The "offset V" osteotomy in hallux valgus reduction. In Jay R (ed): Current Therapy in Podiatric Surgery. Toronto, BC Decker, 1988, pp. 158-161.
12. Patton, G., Zelichoski, J. Proximal Osteotomies for Corrections of Hallux Abducto Valgus with Metatarsus Primus Adductus Deformity in Comprehensive Textbook of Hallux Abductus Valgus Reconstruction, Marcinko, D. (ed.), Mosby Year Book, St. Louis, pp. 147-169, 1992.
13. Mau, C., Die operative Behalung des hallux valgus (Nachunters uchungen). Dtsch Z Chir, 197:361-377, 1926.
14. Ludloff, K. Die Beseitgung des Hallux Valgus dirch die schrage plantodorsale Osteotomei des Metatarsalus I. Arch. Klin. Chir. 110:364-387, 1918.
15. Kitaoka, H., Alexander, I., Adelaar, R., Nunley, J., Myerson, M., Sanders, M. Clinical Rating System for the Ankle-Hindfoot, Midfoot, Hallux and Lesser Toes, Foot Ankle Int., 15:349-353, 1994.
16. Brown, C.W., Orme, T.J., and Richardson, H.D., The rate of pseudoarthrosis (Surgical nonunion) in patients who are smokers and patients who are nonsmokers; A comparison study. Spine, 11:942-943, 1986.
17. Cobb, T.K., Gabrielsen, T., Campbell, D., Wallrich, S. Iltrue, D., Cigarette smoking and nonunion after ankle arthrodesis. Foot & Ankle, 15:64-67, 1994.
18. Haendel, C., Lindholm, J.A., First metatarsal wedge osteotomies. J. Am. Podiatric Med. Assoc., 72:550-556, 1982.
19. Cisar, J., Holz, U., Jenniger, W. Die Osteotomie nach Ludloff bie des Hallux-Valgus-Operation. Akt. Traumatol. 13:247-249, 1983.
20. Blatter, G., Magerl, F. Osteotomien des ersten Strahls zur Behandling des Hallux Valgus. Therapeutische Umschan 48:803-811, 1991.
FIGURE LEGENDS
Figure 1 Ludloff Osteotomy (arrows)
Figure 2 Temporary fixation
Figure 3 Screw fixation (with plantarly medial "overhang")
Figure 4 Remodeled osteotomy
Figure 5 A and B Preoperative weight-bearing anteroposterior and lateral views.
Figure 6 A and B Postoperative anteroposterior and lateral views in same patient that had a Ludloff-Akin procedure. Note osteotomy (arrows).
TABLE 1
| Patient | Date of Surgery | Age/Gender | Procedure | Pre-OpAngles | Post-Op Angles(6 weeks) | Post-Op Angles (months) | AOFAS Scores | Comments |
| 1 | 4/91 | 47/F | Right Ludloff/Akin | IM= 14 HA= 30 MPD=-5 TSP= 6 |
7 16 -7 5 |
(6 mos) 7 15 -8 5 |
90 | *1st met. head cyst *screw removal @ 4 years post-op |
| 2 | 6/91 | 39/F | Right Ludloff | IM= 10 HA= 25 MPD= 0 TSP= 2 |
10 15 -2 1 |
87 | *Metatarsus adductus angle = 28 *1st metatarsal elevatus *2nd MPJ synovitis 4 years post-op |
|
| 3 | 10/91 | 39/F | Left Ludloff | IM= 11 |
8 15 -2 1 |
87 | *Same as above with similar findings | |
| 4 | 7/91 | 65/F | Right Ludloff/ Total Hinged Silicone 1st MPJ implant | IM= 17 HA= 38 MPD=-3 TSP= 6 |
12 20 -6 2 |
(1 year) 10 19 -6 2 |
100 | *Kirschner wire fixation |
| 5 | 12/91 | 57/F | Left Ludloff/ Total Hinged Silicone 1stMPJ implant | IM= 20 HA= 50 MPD=-3 TSP= 7 |
6 5 -3 2 |
(6 mos) 9 11 -3 3 |
95 | |
| 6 | 1/92 | 49/F | Right Ludloff/Akin | IM= 15 HA= 34 MPD=-2 TSP= 7 |
15 12 -4 3 |
72 | *Hypermobile 1st ray *Connective tissue disorder with recurrence of HAV |
|
| 7 | 7/92 | 65/F | Left Ludloff | IM= 15 HA= 21 MPD=+2 TSP= 4 |
10 16 0 2 |
100 | ||
| 8 | 1/93 | 50/F | Left Ludloff/Akin | IM= 20 HA= 34 MPD=-4 TSP= 7 |
11 12 -3 4 |
93 | ||
| 9 | 8/93 | 59/F | Left Ludloff/Akin | IM= 16 HA= 30 MPD=-2 TSP= 7 |
9 7 -4 4 |
95 | ||
| 10 | 2/94 | 32/F | Left Ludloff | IM= 16 HA= 18 MPD= 0 TSP= 5 |
(1 year) 9 12 -1 3 |
100 | *Tailors bunionectomy also performed | |
| 11 | 7/94 | 46/F | Right Ludloff/Akin | IM= 22 HA= 40 MPD=-10 TSP= 7 |
10 15 -12 5 |
83 | Very short 1st metatarsal Lack of hallux purchase | |
| 12 | 9/94 | 26/F | Left Ludloff/Akin | IM= 16 HA= 28 MPD=-3 TSP= 7 |
10 10 -4 3 |
100 | *Metatarsus adductus angle = 20 | |
| 13 | 12/94 | 26/F | Right Ludloff/Akin | IM= 16 HA= 32 MPD=-3 TSP= 6 |
6 8 -3 3 |
100 | *Same patient as above *Metatarsus adductus angle = 24 |
|
| 14 | 11/94 | 57/F | Left Ludloff | IM= 15 HA= 20 MPD=-4 TSP= 4 |
8 20 -6 2 |
(9 mos) 8 20 -6 2 |
90 | *Delayed union that healed at 9 months *Long-term smoker |
Abbreviations: IM, Intermetatarsal; HA, Hallux Abductus; MPD, Metatarsal Protrusion Distance; TSP, Tibial Sesamoid Position; MPJ, Metatarsal Phalangeal Joint; HAV, Hallux Abducto Valgus
AOFAS Score: American Orthopedic Foot and Ankle Society.
TABLE 2
| Average Pre-operative angles |
Average angles at latest post-operative x-ray |
Average reduction | |
| 14 Ludloff procedures All females Average age=47 yrs. Average AOFAS score = 92.3/100 Average followup = 48 months as of 1/97 |
IM= 15.9 HA= 30.1 MPD= -2.7mm TSP= 5.6 |
9.4 13.4 -4.1mm 2.9 |
-6.5 -16.7 < 1.4mm |
Home | About Dr. Saxena | Articles | Appointments | Shoe List | Orthoses
Medial Distal Tibial Syndrome (Shin Splints) | Sever's Disease/Calcaneal Apophysitis
Ankle Sprains & Calf Strains | Injury Prevention | Heel Pain | Achilles Heel | Ankle Stretching, Rehabilitation & Taping
Return to Sports After Injury | Cycling | Marathons | Videos | Recommended Books | Links
Friends & Patients | Legal Notice | Privacy Statement | Site Map
Copyright © Amol Saxena, DPM - Sports Medicine & Surgery of the Foot & Ankle
Web Site Design, Hosting & Maintenance By Catalyst Marketing Innovations, LLC/ Worry Free Websites