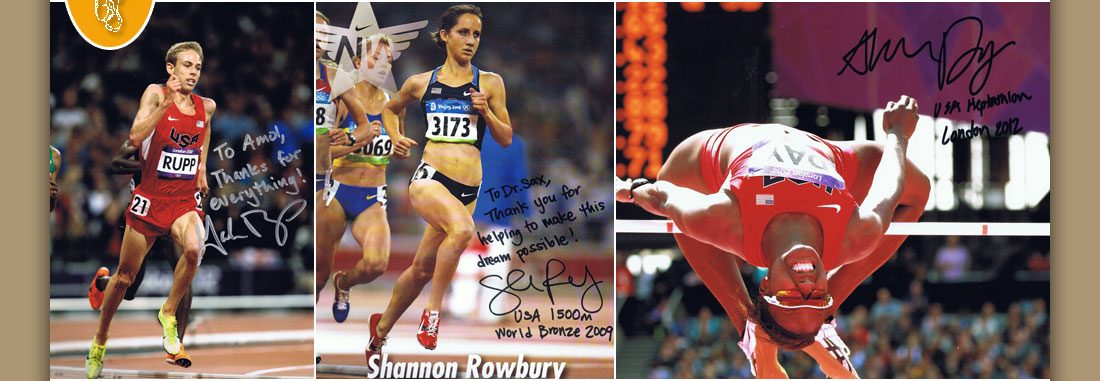

Dr. Amol Saxena, DPM
Palo Alto Foundation
Medical Group
Dept. of Sports Medicine
3rd Floor, Clark Building
795 El Camino Real
Palo Alto, CA 94301
Office: 650-853-2943
Fax: 650-853-6094
E-Mail
Map | Directions

| Articles |
The Valenti Procedure for Hallux Limitus/Rigidus
Amol Saxena, DPM, FACFAS
Dept. of Sports Medicine
Palo Alto Medical Foundation
913 Emerson St.
Palo Alto, CA 94301
Published in the Journal of Foot And Ankle Surgery Vol 5 1995.
UPDATE ON THE VALENTI PROCEDURE: My follow-up of 27 procedures reveals Good to Excellent Results in 21 cases, Fair in 2, and 4 were lost to follow-up. These results compare favorably to other procedures done for Hallux Rigidus. Unfortunately, few Doctors on the West Coast perform this procedure, which is very popular in the Midwest and parts of the East. (I’m not sure why, as I’ve found people’s feet are the same no matter which part of the US you live in.)
ABSTRACT
The results of twelve Valenti procedures on eleven patients are presented. Pre-operative Hallux dorsiflexion was 12.9 degrees; post-operatively patients achieved 40.4 degrees of dorsiflexion. The Valenti procedure is a useful arthroplasty for Grades II and III Hallux Limitus/Rigidus.
Orthopaedic and Podiatric literature is repleat with surgical procedures to address hallux limitus/rigidus. The most common procedures include cheilectomy, the Keller procedure, implant arthroplasty, and arthrodesis. Multiple osteotomies have also been described including the Regnauld, Waterman, and Bonny-Kessel to treat this deformity.(1-18) Varying degrees of success of these procedures have been noted, and silicone implants have been cited for many complications.(19,20,21)
Normal hallux dorsiflexion is 45 to 65 degrees, with respect to the weightbearing plane.(22) Less than 20 degrees of dorsiflexion indicates pathology due to limited first metatarsophalangeal joint range of motion.
Hallux limitus/rigidus is classified in four stages(23):
GRADE I - Known as a functional hallux limitus which involves little joint adaptation and degenerative deformity, yet hallux dorsiflexion is limited in gait.
GRADE II - Consists of early joint adaptation with boney hypertrophy and a decrease in dorsiflexion even with non-weightbearing.
GRADE III - Consists of further joint deterioration and arthrosis with hallux dorsiflexion generally less than 10 degrees.
GRADE IV - Essential loss of joint space. Boney ankylosis/fusion of the first metatarsophalangeal joint may occur.
The etiology of hallux limitus/rigidus is often attributed to hypermobile first ray, which may result in a functional hallux limitus, which is defined as less than 20 degrees of hallux dorsiflexion in gait. (22,23) Variation in first metatarsal and first proximal phalanx length and shape are also contributing factors. Other biomechanical abnormalities resulting in increased pronation at midstance and toe off are correlated with hallux limitus/rigidus. (22,23,24) Repetitive trauma to the first metatarsophalangeal joint may cause this deformity. Long- standing metabolic conditions such as rheumatoid arthritis and gout are also implicated in the formation of hallux limitus/rigidus.(24)
In 1976, Valente Valenti, an Italian orthopaedic foot surgeon, began performing a sagittal plane "V" resection of the first metatarsophalangeal joint for hallux limitus/rigidus. (personal communication) The resection involved preservation of the plantar portion of the first metatarsal head and first proximal phalanx base, thereby preserving the flexor hallucis brevis insertion and sesamoid function. His technique and results were first presented at the 1987 Hershey Seminar in Pennsylvania. The current technique has been performed by this author since 1988 and the preliminary results of 12 cases are presented in this paper.
OPERATIVE TECHNIQUE
A dorsal/medial linear incision is made over the first metatarsophalangeal joint. A linear capsulotomy is performed and hypertrophic synovium/bursal tissue is sharply excised. A power saw is used to resect the dorsal and medial metatarsal eminences. The lateral eminence, if present, may be resected if appropriate. Inspection of the articular surfaces is next performed, examining for osteochondral defects. Usually Grade III and Grade IV hallux limitus rigidus have a significant degree of articular cartilage loss.(Fig. 1 ) The metatarsal "osteotomy" is next performed, first extending from dorsal proximal to plantar distally extending below the degenerated articular cartilage. Usually the dorsal half to two-thirds of the metatarsal head is removed, preserving the sesamoid articulation with the Crista.(Fig. 2A & B) One should take note that in hallux rigidus, the Crista extends dorsally and the osteotomy/resected bone may appear to be greater than it actually is.
The next step involves the osteotomy of the proximal phalanx, again resecting a greater portion dorsally than plantarly. Preservation of the flexor hallucis brevis insertion is paramount. Generally, the extensor hallucis brevis is released with this resected portion of bone of the proximal phalanx. As with other hallux limitus/rigidus procedures, the extensor hallucis longus tendon may be lengthened if appropriate. A metatarsal head deglover/elevator is used to mobilize the typically adhered sesamoids. The remaining synovium of the first metatarsophalangeal joint should be hour-glassed or alternatively, a dorsal flap of synovium can be sewn down onto the metatarsal head. Wound closure is done in the preferred fashion. Occasionally, a drain is inserted, and then removed 1-2 days postoperatively.(Fig. 3)
POSTOPERATIVE PROTOCOL
Weightbearing to tolerance and a flexible surgical shoe is permitted immediately. Active hallux range of motion is then initiated, though the bulky compressive dressing may limit motion. Suture removal is done in seven to ten days. Physical therapy including electrical and muscle stimulation, contrast baths, and range of motion exercises are instituted at ten days to three weeks postoperatively, and courses for two to three weeks, two to three times a week. The patients are permitted to use open toed sandals or shoes after suture removal. A progression to athletic and dress shoes (usually by 3-8 weeks) is based on tolerance and edema. For the athletic patient, biking is permitted one to two days postoperatively. Swimming is allowed after suture removal. Running is generally allowable in three to six weeks, depending on the patients range of motion, edema, discomfort, and ability to fit in shoes.
RESULTS
Twelve procedures were performed on eleven patients, (7 females and 4 males). The average patient age was 45.6 years (Range 39-54) with an average postoperative follow-up of 21.1 months. Classification values for the degree of hallux limitus/rigidus (one equals Grade I, two equals Grade II, etc) was done. The average grade of hallux limitus/rigidus was 2.42. There was only patient classified as a Grade IV and no Grade I's. The average preoperative duration of symptoms was 8.3 years and most had tried functional orthoses, physical therapy, and non-steroidal anti-inflammatory medications or some combination of the above. Preoperative average dorsiflexion and plantar flexion was measured with respect to the weight bearing surface and found to 12.9 degrees and 5.8 degrees, respectively.(Fig. 4) Postoperative values yielded at an average of 40.4 degrees of dorsiflexion and 6.8 degrees of plantar flexion.(Fig. 5) This resulted in a 27.5 degrees increase in dorsiflexion. The range of postoperative dorsiflexion was 20-70 degrees. The combined angle of the osteotomy in the sagittal plane was 50.7 degrees.(Fig. 6) Six patients were judged to have "excellent" results, three "good", one "fair," and one "poor." (This last patient had bilateral procedures and hypothyroidism, possibly resulting in greater pedal edema.) Two patients had a lack of toe purchase, however, one did not have toe purchase preoperatively. One patient developed a suture abscess. Three patients, all with plantarflexed first rays, had transient sesamoiditis, which gradually resolved with the use of orthoses or temporary foot padding. Intraoperatively, two patients who had previous trauma were found to have a torn extensor hallucis longus tendon.
DISCUSSION
The Valenti procedure allows for increased dorsiflexion, and removal of the degenerated portion of the first metatarsophalangeal joint. There is essentially no shortening of the hallux and the flexor hallucis brevis attachment is maintained, thereby preserving push-off strength. These are common failures of the Keller procedure. (13,14) This procedure when performed with the osteotomy angle at 45 degrees each, giving a combined osteotomy of 90 degrees would theoretically allow for 90 degrees of dorsiflexion. (Refer to Fig. 6) This author could not correlate an increase in postoperative dorsiflexion the closer the combined osteotomy angle got to 90 degrees.
Though the Valenti procedure involves resecting a large portion of the joint, there is still adequate bone remaining to allow for an implant, should it be needed at a later date. In some cases, the patients may not be able to form adequate replacement fibrocartilage and the exposed chondral bone may result in pain in end-range dorsiflexion. Also, the patient with a plantarflexed first ray may be more prone to develop sesamoiditis postoperatively. This is due to the increased ability to dorsiflex the hallux, allowing for greater plantarflexion of the first metatarsal.
CONCLUSION
The Valenti procedure has been found to successfully increase hallux dorsiflexion and decrease pain in patients with Grade II and III hallux limitus/rigidus. The procedure avoids placing implant in a middle aged patient, preserves intrinsic muscle function and allows immediate weightbearing. The patients gain on average 27.5 degrees of dorsiflexion postoperatively. Functional return to athletic activities is usually by six weeks, postoperatively.
REFERENCES
1. Vanore, J. V., Corey, S. V. Hallux Limitus Rigidus and Metatarsophalangeal Joint Arthrosis. in Comprehensive Textbook of Hallux Abduct Valgus Reconstruction. pp. 209-242 Edited by D.E. Marcinko, Mosby Year-book, St. Louis, 1992.
2. Calderone, D. R., Wertheimer, S. J. First metatarsophalangeal joint arthrodesis utilizing a mini-Hoffman External Fixator. J. Foot Ankle Surg 1993 Sep-Oct; 32 (5):517-25.
3. Blair, M. P., Brown, L. A. Hallux limitus/rigidus deformity: a new great toe implant. J Foot Ankle Surg 1993 May-Jun; 32 (3):257-62.
4. Cohen, M., Roman, A., Liessner, P. A modification of the Regnauld procedure for hallux limitus. J Foot Surg 1992 Sep- Oct; 31 (5):498-503.
5. Smith, R. W., Joanis, T. L., Maxwell, P. D. Great toe metatarsophalangeal joint arthrodesis: a user-friendly technique. Foot Ankle 1992 Sep; 13 (7):367-77.
6. Barouk, L. S. Osteotomies of the great toe. J Foot Surg 1992 Jul-Aug; 31 (4):388-99.
7. Feldman, K. A. The Green-Watermann procedure analysis and preoperative radiographic template technique. J Foot Surg 1992 Mar-Apr; 31 (2):182-5.
8. Geldwert, J. J., Rock, G. D., McGrath, M. P., Mancuso, J. E. Cheilectomy: still a useful technique for grade I and grade II hallux limitus/rigidus. J Foot Surg 1992 Mar-Apr; 31 (2):154-9.
9. Hanft, J. R., Kashuk, K. B., Toney, M., Schabler, J. Modifications of the Regnauld osteochondral autogenous graft for correction of hallux limitus/valgus: a 2-year review. J Foot Surg 1992 Mar-Apr; 31 (2):116-9.
10. Cracchiolo, A. 3d, Weltmer, J. B. Jr, Lian, G., Dalseth, T., Dorey, F. Arthroplasty of the first metatarsophalangeal joint with a double-stem silicone implant. Results in patients who have degenerative joint disease failure of previous operation, or rheumatoid arthritis. Comment in: J Bone Joint Surg Am 1993 Aug: 75 (8):1254-5, J Bone Joint Surg Am 1992 Apr; 74 (4):552-63.
11. Shankar, N. S., Asaad, S. S., Craxford, A. D. Hinged silastic implants of the great toe. Clin. Orthop. 1991 Nov; (272):227-34.
12. Hanft, J. R., Feiertag, M. A., Schabler, J. A., Janecki, C. J., Kashuk, K. B. Preliminary report: modification of the Regnauld osteochondral autogenous graft. J Foot Surg 1990 Nov-Dec; 29 (6):577-80.
13. O'Doherty, D. P., Lowrie, I. G., Magnussen, P. A., Gregg, P. J. The management of the painful first metatarsophalangeal joint in the older patient. Arthrodesis or Keller's arthroplasty? J Bone Joint Surg (Br) 1990 Sep; 72 (5):839-42.
14. Quinn, M., Wolf, K., Hensley, J., Kruljac, S. Keller arthroplasty with autogenous bone graft in the treatment of hallux limitus. J Foot Surg 1990 May-Jun; 29 (3):284-91.
15. McAuliffe, T. B., Helal, B. Replacement of the first metatarsophalangeal joint with a silicone elastomer ball-shaped spacer. Foot Ankle 1990 Apr; 10 (5):257-62.
16. Davies, G. F. Plantarflexory base wedge osteotomy in the treatment of functional and structural metatarsus primus elevatus. Clin Podiatr Med Surg 1989 Jan; 6(1):93-102.
17. DeLauro, T. M., Positano, R. G. Surgical management of hallux limitus and rigidus in the young patient. Clin Podiatr Med Surg 1989 Jan; 6 (1):83-92.
18. Broughton, N. S., Doran, A., Meggitt, B. F. Silastic ball spacer arthroplasty in the management of hallux valgus and hallux rigidus. Foot Ankle 1989 Oct; 10 (2):61-4.
19. Verhaar, J., Bulstra, S., Walenkamp, G. Silicone arthroplasty for hallux rigidus. Implant wear and osteolysis. Acta Orthop Scand 2989 Feb; 60 (1):30-3.
20. Freed, J. B. The increasing recognition of medullary lysis, cortical osteophytic proliferation, and fragmentation of implanted silicone polymer implants.
21. Rahman, H., Fagg, P. S. Silicone granulomatous reactions after first metatarsophalangeal hemiarthroplasty. J Bone Joint Surg Br 1993 Jul; 75 (4):637-9.
22. Root, M.L., Orien, W.P., Weed, J.H. Clinical Biomechinics - Volume II Normal and Abnormal Function of the foot. Clinical Biomechanics Corp., Los Angeles, 1977
23. Hanft, J. R., Mason, E. T., Landsman, A. S., Kashuk, K. B. A new dradiographic classification for hallux limitus. J Foot Ankle Surg 1993 Jul-Aug; 32 (4):397-404.
24. Clayton, M. L., Ries, M. D. Functional hallux rigidus in the rheumatoid foot. Clin Orthop 1991 Oct; (271):233-8.
Valenti Figure Legends
Fig. 1: Full thickness articular cartilage loss in the 1st MPJ.
Fig. 2A&B: Same patient as in Fig. 1 with Pre- and Post- operative X-rays 2A & 2B respectively.
Fig. 3: AP View of previous patient with drain inserted.
Fig. 4: Pre-operative Data.
Fig. 5: Post-operative Results.
Fig. 6: Valenti Osteotomy angle - the angular relationship in the sagittal plane of the resected bone surfaces.
Home | About Dr. Saxena | Articles | Appointments | Shoe List | Orthoses
Medial Distal Tibial Syndrome (Shin Splints) | Sever's Disease/Calcaneal Apophysitis
Ankle Sprains & Calf Strains | Injury Prevention | Heel Pain | Achilles Heel | Ankle Stretching, Rehabilitation & Taping
Return to Sports After Injury | Cycling | Marathons | Videos | Recommended Books | Links
Friends & Patients | Legal Notice | Privacy Statement | Site Map
Copyright © Amol Saxena, DPM - Sports Medicine & Surgery of the Foot & Ankle
Web Site Design, Hosting & Maintenance By Catalyst Marketing Innovations, LLC/ Worry Free Websites