
Dr. Amol Saxena, DPM
Palo Alto Foundation
Medical Group
Dept. of Sports Medicine
3rd Floor, Clark Building
795 El Camino Real
Palo Alto, CA 94301
Office: 650-853-2943
Fax: 650-853-6094
E-Mail
Map | Directions

| Foot Related Injuries & Treatments |
Heel Pain
Heel pain accounts for over 20% of patient visits to foot specialists and a third of all patient visits I see. Over 50% of Americans will experience heel pain during their lifetime. The most common form of heel pain is known as Plantar Fasciitis or “Heel Spur Syndrome”. The Plantar fascia is a thick ligament on the bottom of your foot spanning from your heel to the base of your toes. It supports the arch and several muscles under the bones that support the foot. Overtime, most people will develop some degree of calcification within these muscles on the bottom of their heel, which is called a “spur” but is entirely innocuous. Hence, the term “Heel Spur Syndrome” is a misnomer.
Plantar Fasciitis is a condition of irritation to the Plantar Fascia, the thick ligament on the bottom of your foot. It classically causes pain and stiffness located on the bottom of your heel and feels worse in the morning with the first steps out of bed and also in the beginning of an activity after a period of rest. For instance, after driving a car, people feel pain when they first get out, or runners will feel discomfort for the first few minutes of their run. This occurs because the Plantar Fascia is not well-supplied by blood (which makes this condition slow in healing) and a certain amount of activity is needed to get the area to warm up. Plantar Fasciitis can occur due to various reasons: use of improper, non-supportive shoes, over-training in sports, lack of flexibility, weight gain, prolonged standing and interestingly, prolonged bed-rest.
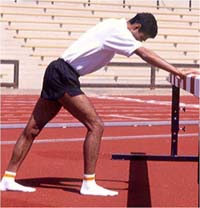
Treatment initially is adding support to the foot including better shoes and an over-the-counter arch support/insole, resting from the sport or activity exacerbating it, stretching the calf and arch muscles, and anti-inflammatories including ice and massage. The latter two can be accomplished simultaneously by taking a filled water bottle, freezing it solid & then using the now frozen ice cylinder, to massage your foot for 5-10 minutes by rolling it underneath at least two times per day (see below). It is not unusual for symptoms of Plantar Fasciitis to persist for 6-12 months despite trying the myriad of treatment options.
 Plantar Fascia Stretch Hold for 15 seconds & perform before getting out of bed, before and after exercise and before night-time icing |
 Arch Tape |
 Plantar Fascia Icing Roll of frozen cylindrical frozen water-bottle after exercise and before bed for 5-10 minutes |
Other treatment considerations for Plantar Fasciitis include custom prescription foot orthoses (“orthotics”), weight loss when indicated, steroid injections and /or physical therapy to decrease the inflammation, night-splints and/or cast boots to splint and limit the stress on the Plantar Fascia. Another, relatively new modality is Orthotripsy (high frequency ultra-sonic shock-waves) which has been shown to decrease the pain significantly in 50-85% of patients in the studies published. Surgery (which can be done endoscopically) is usually not needed for over 90% of the cases of Plantar Fasciitis, but when indicated is about 85% successful. Patients who are overweight do not seem to benefit as much from surgery. Generally, Plantar Fasciitis is a condition people learn to control.
There are a few “Plantar Fascia-like” conditions one should be aware of. The most common occurs acutely: the patient continues to exercise despite the symptoms and experience a sudden sharp pain on the bottom of the heel, with the inability to stand on their toes and subsequent bruising in the arch. This is a rupture of the Plantar Fascia and is treated very successfully by immobilization in a cast boot for 2-6 weeks, a period of active rest and physical therapy. Another problem with prolonged and neglected Plantar Fasciitis is development of a stress fracture from the constant traction of this ligament on the heel bone. This appears more common in osteoporotic women, and is also treated with cast boot immobilization. The nerves that course along the heel occasionally get inflamed by the subsequent thickening and inflammation of the adjacent Plantar Fascia. These symptoms often feel like numbness and burning and usually resolve with physical therapy and injections. One should also be aware that heel numbness can be the first sign of a back problem.
The Achilles tendon (the cord-like structure attaching your calf muscle to your heel) is another region where heel pain is common. The Achilles tendon can be injured acutely, known as a rupture, which when completely severed, usually is repaired surgically which is very successful. (Partial ruptures usually are not repaired surgically but if they are not protected with a period of immobilization, can be limiting and chronic.) Patients sustaining a rupture usually experience a “pop” in the back of their heel and cannot support their weight on one limb while rising up on their toes. Basketball and tennis are the most common culprits. Recovery usually takes 6-12 months.
 |
 |
The Achilles tendon can also get inflamed chronically known as Tendonosis. Sometimes this is due to microscopic tears within the tendon or previous partial tears that were not rested and rehabilitated properly. The symptoms are similar to Plantar Fasciitis in that stiffness and pain is worse in the morning and initial portions of activity. Lumps or swelling, along with a burning sensation are signs that activities should be stopped to avoid exacerbating the condition and possibly creating a rupture. Certain medications such as oral steroids and a class of antibiotics known as Quinolones increase the potential of Achilles Tendonosis and rupture. Initial treatment includes rest, use of heel cushions to elevate the heel (and take tension off the Achilles), stretching (see above) and icing. These latter two can be done simultaneously by filling a bucket with cold water and a tray of ice cubes and place the foot flexed with the toes upward so that the Achilles tendon region is bathed in the cold water for 10-15 minutes twice a day (see above).The Achilles region can also get inflamed around the tendon called Paratendonosis. This can be treated with the ice bucket stretching, rest and physical therapy. Another area that is commonly subjected to problems is the attachment of the Achilles near or on the heel bone. The heel (calcaneus) itself can have an irregular shape to it causing irritation to the Achilles as it twists over the region, inflaming the “bursa”, a naturally occurring cushion. Shoes can often aggravate this. Sometimes over-stretching such as the Achilles stretch with the knee bent can irritate the tendon and cause a bursitis as well. Prescription foot orthoses can help reduce the torque of the Achilles tendon in these types of cases.
Often the Achilles tendon calcifies near it’s attachment due to constant torque and tension. Repetitive stress can cause this calcific spur to crack creating a chronic inflammatory situation that can require surgery. All of these types of chronic Achilles Tendonosis that require surgery are successfully treated in over 90% of the cases; though complete recovery, as with most foot surgery can take up to a year. Though heel pain is prevalent and can be chronic, it does not have to be your weakness as was the case with the warrior Achilles from Greek mythology.

Sample Charges
Sample charges in US$ from 12 orthopedic and podiatric offices for treatment of plantar fasciopathy & Achilles tendinopathy nationwide (excluding radiological exams) typically incurred by patients before considering soundwave, surgery, etc.
Dr. office visits (initial and 2+ follow-up) - $700+
Physical Therapy (minimum 6 visits) - $1200+
Over-the-counter inserts & night splint - $60+
NSAIDS (OTC & Rx) - $15+
Custom Orthoses - $350+
Cortico-steroid Injection (generally not applicable for Achilles) - $250+
TOTAL - $2560+
Adapted from: Saxena, A, Fullem, B “Plantar Fascial Injuries” in Foot and Ankle in Sports Medicine ( editors: David W. Altchek, M.D., Jonathan T. Deland, M.D., Christopher DiGiovanni, M.D.,Rock G. Positano, DPM, MSC, MPH, and Joshua Dines, M.D.) Lippincott 2012
Summary of Benefits
Summary of benefits of current treatment options for Plantar Fasciopathy:
| PHASE 1: | |
| Stretching of calf and arch | High Level Evidence |
| Over-the counter arch supports | Medium Level Evidence |
| Cryotherapy | Medium Level Evidence |
| Night splints | Medium Level |
| NSAIDS | Low Level (unless inflammatory arthropathy) |
| Physical Therapy (UltrasoundS & Iontophoresis) | Low Level |
| PHASE 2: | |
| ESWT/Soundwave | High Level Evidence |
| Custom Orthoses | Medium Level Evidence |
| Cortico-steroid injection | Medium Level Evidence |
| Platelet Rich Plasma(PRP/ABI) | Low Level |
| SURGERY: | |
| Endoscopic Plantar Fasciotomy | High and Medium Level Evidence |
| Open and Percutaneous Fasciotomy | Low Level |
| Gastrocnemius recession | Low Level |
| TOPAZ | Low Level |
| Experimental/Under-reported therapies | LASER, Acupuncture, Needling, massage |
Adapted from: Saxena, A, Fullem, B “Plantar Fascial Injuries” in Foot and Ankle in Sports Medicine ( editors: David W. Altchek, M.D., Jonathan T. Deland, M.D., Christopher DiGiovanni, M.D.,Rock G. Positano, DPM, MSC, MPH, and Joshua Dines, M.D.) Lippincott 2012
Home | About Dr. Saxena | Articles | Appointments | Shoe List | Orthoses
Medial Distal Tibial Syndrome (Shin Splints) | Sever's Disease/Calcaneal Apophysitis
Ankle Sprains & Calf Strains | Injury Prevention | Heel Pain | Achilles Heel | Ankle Stretching, Rehabilitation & Taping
Return to Sports After Injury | Cycling | Marathons | Videos | Recommended Books | Links
Friends & Patients | Legal Notice | Privacy Statement | Site Map
Copyright © Amol Saxena, DPM - Sports Medicine & Surgery of the Foot & Ankle
Web Site Design, Hosting & Maintenance By Catalyst Marketing Innovations, LLC/ Worry Free Websites