
Dr. Amol Saxena, DPM
Palo Alto Foundation
Medical Group
Dept. of Sports Medicine
3rd Floor, Clark Building
795 El Camino Real
Palo Alto, CA 94301
Office: 650-853-2943
Fax: 650-853-6094
E-Mail
Map | Directions

| Articles |
Surgery for Chronic Achilles Problems.
Published in the Journal of Foot And Ankle Surgery Vol 3 1995.
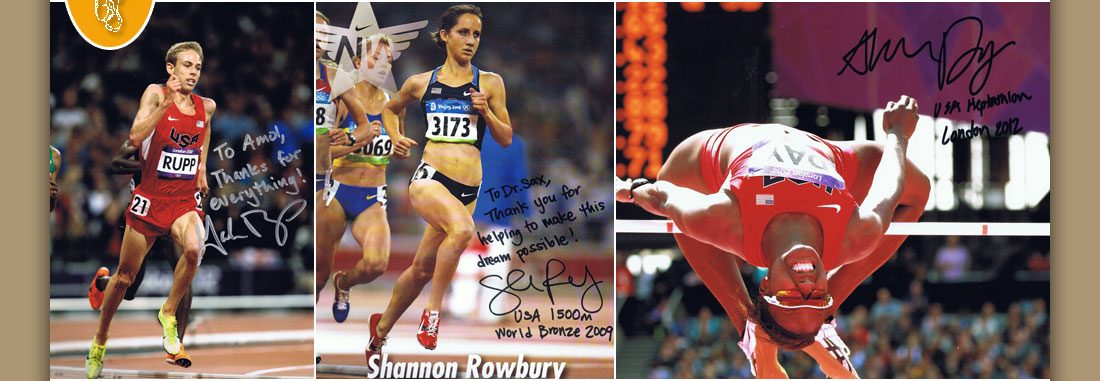
UPDATE ACHILLES: I have now had 65 patients undergo various Achilles procedures, with 90% having Good to Excellent results. This compares favorably to Schepsis & Leach’s paper in 1994 Am. Journal of Sports Medicine, where they presented the results of 79 surgeries done over 13 yrs; they had an 85% success rate. I have had the opportunity to operate on National & Olympic Champion’s achilles, and though it’s generally successful, it should not be taken lightly. I’m still finding various pearls and will be presenting additional research info at upcoming meetings.
ABSTRACT
The author introduces a new procedure for surgical treatment of Achilles tendocalcinosis. In addition, other techniques are presented for treatment of various chronic Achilles pathology. Results of 21 procedures on 19 patients are presented.
Achilles tendon pathologies can encompass multiple entities. William's classifies them into: rupture, focal degeneration, tendinitis, peritendinitis (peritendinosis), mixed lesions, origin/insertion lesions, and other cases such as metabolic/rheumatic causes. (1) Etiologies include trauma, poor flexibility and abnormal body mechanics (such as excessive pronation or supination and limb length inequalities). (1-7)
The anatomy of the Achilles is different from the other tendons inserting into the foot. It lacks a true synovial sheath and has a paratenon covering instead. Due to the decreased vascularity, the Achilles tendon is particularly vulnerable at its "watershed" region which is 2 to 6 centimeters proximal to its insertion. (8) Achilles peritendinosis involves inflammation of the peritendinous tissues (the paratenon). Achilles tendinosis may consist of focal degenerative changes of the Achilles tendon itself. In chronic conditions, this may result in mucoid or fatty degeneration of the Achilles tendon. (9,10)
Differentiating between peritendinosis and Achilles tendinosis may be confusing, as often with chronic Achilles problems, both may co-exist. (1,2,4,5,10,11) Clinically, peritendinosis manifests itself as peritendinous crepitus as the Achilles tries to glide within the inflamed covering. (2,3,7) The patient's symptoms often increase with activity. Diffuse swelling and fibrosis along the length of the watershed region may be noted. In contrast, tendinosis (tendinitis) symptoms tend to decrease with activity; fibrosis and tenderness is more localized. (2,4,11) Some cases of tendinosis may be associated with previous partial or complete rupture. (1)
Tendocalcinosis involves calcification of the Achilles tendon insertion, though calcification may occur in other regions. Proximal, posterior or distal to the calcifications, symptoms such as tendinosis and bursitis may occur. (1,12) In addition, a prominent posterior superior calcaneus (Haglund's deformity) may also result in posterior heel pain and be a coexisting deformity. (4,6,11,13) Symptoms include localized pain and a posterior superior prominence resulting in symptomatic bursitis and retro-Achilles tenderness.
Evaluation of Achilles pathology includes the traditional weightbearing and non-weightbearing exam including neurovascular status. A biomechanical evaluation, especially ankle range of motion, is performed. Radiographic examination utilizing plain film radiography is mandatory. In addition, xerograms, bone scans and MRIs may be appropriate. Conservative treatment includes combinations of rest, anti-inflammatories, physical therapy, heel lifts, accommodative padding and functional orthosis. (2,3,5,7) Some authors report patients receiving relief from acupuncture and dimethyl sulfoxide (DMSO).(1,3) Surgical treatment involves tenolysis, tendon repair and excision of calcinosis or other prominences/bursae, and tenodesis as appropriate. (2,7,11,14,15) The purpose of this paper is to present various surgical techniques and postoperative protocols for peritendinosis, tendinosis and tendocalcinosis/tenodesis.
Surgical techniques
I. Tenolysis of peritenon (decompression of the Achilles tendon). A linear incision paralleling the Achilles tendon is used on the side of greatest pathology. Care is taken to avoid the sensory branches of the tibial nerve medially and sural nerve laterally. The abnormal fibrotic tendinous tissue is excised.(Fig. 1A & B) Often times, the paratenon will have a transparent mucinous appearance and deep to it will lie focally degenerated abnormality within the tendon.(Fig. 2) This area is curetted and excised. Repair of the defect is done with #3-0 absorbable suture. After medial, lateral and dorsal tenolysis is carried through and the Achilles tendon is thoroughly decompressed, only subcutaneous tissue and skin are reapproximated. A buried knot #3-0 absorbable suture is used for subcutaneous tissues and #4-0 monofilament polypropylene suture is used subcuticularly for skin.
Postoperatively, the patient is kept non-weightbearing for 1 1/2 to 3 weeks in a posterior splint (depending on the amount of focal degeneration involved). The patient progresses to partial and then full weightbearing over the next 1 1/2 to 4 weeks. Physical therapy is initiated 2-6 weeks (consisting of electrical stimulation, contrast baths, range of motion and isokinetic exercises). Gradual resumption of running sports is allowed at 4-8 weeks postoperatively.
Procedure II. Tendinosis excision/repair
For those patients that have a large area of intra-tendonous mucoid degeneration,(Fig. 3A & B) a similar paralinear incision is made centering over the nodular fibrosis. The degenerated paratenon is excised and then the nodularly thickened portion of the tendon is linearly incised. Excision of the mucoid material that lies intratendously is carried through.(Fig. 4) The normal appearing white linear Achilles tendon fibers are often not present in this region of nodular fibrosis; instead yellowish, soft, degenerative fibers occupy this region and are therefore excised.(Fig. 5) The remaining Achilles tendon is repaired by using #2 nonabsorbable braided polyester suture in a buried knot fashion. Partial ruptures, if encountered are repaired in a modified Bunnell's manner. Subcutaneous tissue and skin are closed in the same manner as with the tenolysis procedure.
The postoperative care consists of 3-4 weeks non-weightbearing in equinus positioned, below knee cast. A gradual progression of partial to full weightbearing in a below knee cast (walker-type) boot occurs over the next 4 weeks. Physical therapy is started at 8-10 weeks postoperatively and resumption of running sports occurs at 12-16 weeks postoperatively.
Procedure III. Tenocalcinosis and Achilles tenodesis
A modified lazy "S" is incorporated to visualize the posterior superior lateral aspect of the calcaneus and the Achilles tendon insertion inferiorly.(Fig. 6A & B) The incision course is proximal-lateral above the heel, swings midline, and extends inferiorly to the junction of the calcaneal fat pad. For those patient's whose tenocalcinosis involves little to no portion of the Achilles tendon insertion, a simple midline incision can be made to extract the exostosis and associated bursa. This is also done with the lazy "S" incision, however, an osteotome is used to aid and excise in the exostosis from the Achilles tendon insertion. In addition, the proximal lateral portion of the incision allows removal of a Haglunds deformity and retro calcaneal bursa if needed. The Achilles fibers are reflected from the exostosis after it is excised.(Fig. 7A & B) A burr and rasp may be used to remodel the "step" deformity. To aid in tenodesis Mitek G II Quick Anchors* * are placed into the calcaneus.(Fig. 8A, B & C)
The tendon is repaired side to side, and then modified Bunnell fashion using #II nonabsorbable braided polyester suture.(Fig. 9 -Drawing) Subcutaneous tissue and skin are repaired as noted in the previous descriptions.
Postoperative care involves 4 weeks of non-weightbearing in a equinus non-weightbearing cast, followed by 4-6 weeks of partial weightbearing to full weightbearing at a BK cast walker boot. Physical therapy is started at 10-12 weeks postoperatively and resumption of running sports is allowed at 12-20 weeks, depending on the degree of tenodesis required.
RESULTS
Nineteen patients (16 males and 3 females) underwent 21 procedures for Achilles tendon and related pathologies. The average patient age was 46.5 years (One should note the average age of the patients undergoing peritenolysis was 30.2 years.) The average length of symptoms and conservative treatment was 4.3 and 2.6 years, respectively. Five procedures involved peritenolysis, and four others consisted of mucoid degeneration of the Achilles tendon excision. In addition, twelve patients had treatment for tendocalcinosis; nine patients necessitated tenodesis. Among this group of 19 patients were three sub-four minute milers and one eight-time National Cross-country Champion; the remaining patients were all athletically active in either running, tennis, basketball or exercise walking. All of the patients returned to performing daily activities without pain and eighteen out of nineteen returned to their desired level of athletic activities. The peritenolysis group were able to resume running activities on an average of four weeks postoperatively. This differs significantly from the remaining patients who had more involved procedures; these patients returned to their desired activity on the average of fourteen weeks post- operatively.
One patient that had excision of tendocalcinosis and bursa redeveloped a retrocalcaneal bursitis one year later; recommendation was made to have the posterior/superior aspect of the calcaneous and bursa excised. Only two other minor complications were noted; suture irritation from a knot of braided polyester suture, and a superficial wound infection which resulted in a hypertrophic scar on a patient that could not be full non-weightbearing due to scoliosis.
DISCUSSION
Authors have noticed varying degress of success for surgery for chronic Achilles problems. (2,3,4,6,11,13,15) All but one of the patients in this relatively small series did well. The advent of soft tissue anchors appears to decrease the morbidity previously associated with tenodesis. It should be noted that one patient in the tenodesis group previously had a steroid injection for retrocalcaneal bursitis and subsequently suffered an avulsion type rupture of the Achilles insertion.
Previous studies have tried to implicate foot type with Achilles tendonopathies, yet in this study there is no predominence of a pronated nor supinated foot. (1,2,5,7) All patients, however, did have decreased ankle joint dorsiflexion which was measured with the foot in the supinated position. It is debatable that this decrease in ankle dorsiflexion may not necessarily be the cause of the pathology but possibly the result. The reader is referred to Table 1 for the findings with each particular patient.
CONCLUSION
Surgical treatment for Achilles peritendinosis, mucoid degnerated Achilles tendons and tendocalcinosis can be undertaken with the above surgical techniques described. The modified lazy-S incision used offers better exposure to the surgical pathology associated with achilles tendocalcinosis. Adherence to the postoperative protocols allows patients to return to their desired activity level. Prior to undergoing surgery, adequate conservative treatment should be administered. One should note that in this series patients averaged 2.6 years of conservative treatment. When indicated, surgery performed for chronic Achilles tendonopathies is successful.
ACKNOWLEGMENTS
The author wishes to acknowlege Susan Keller for providing the drawings and Drs. D. Bunce, G. Campbell and S. Osborn for the assistance and incorporation for some of the cases presented.
REFERENCES
1. Williams, J. G. Achilles tendon lesions in sports. Sport Med. 3:114-135, 1986.
2. Clement, D. B., Taunton, J. E., Smart, G. W. Achilles Tendinitis and Peritendinitis: Etiology and treatment. Am. J. Sport Med. 12:179-184, 1984.
3. Saxena, A. Achilles Peritendonosis: An unusual case due to frostbite in an elite athlete. J. Foot & Ankle Surg. 1(33):87-90, 1994.
4. Leach, R. E., James, S., Wasilewski, S. Achilles tendinitis. Am. J. Sport Med. 9:93-98, 1981.
5. Galloway, M. T., Jokl, P., Dayton, D. W. Achilles tendon overuse injuries. In Clinics in Sports Medicine, pp.771-782, edited by P. Renstrom and Wayne Leadbetter, W. B. Saunders Co., Philadelphia, 1992.
6. Nelen, G., Martens, M., Burssens, A. Surgical treatment of chronic Achilles tendinitis. Am. J. Sport Med. 17:754-759, 1989.
7. Lemm, M., Blake, R. L., Colson, J.P., Ferguson, H. F. Achilles Peritendinitis. A Literature review with Case Report. J. A. P. M. A. 82:482-490, 1992.
8. Hume, E. L. Traumatic disorders of the ankle or overuse syndromes. In Traumatic Disorders of the Ankle, pp 56-58, edited by W. C. Hamilton, Springer Verlag, New York, 1984.
9. Kvist, M., Jarvinen, M. Clinical histochemical and biomechanical features in repair of muscle and tendon injuries. Int. J. Sport Med. 3 (Suppl) 1:12-14, 1982.
10. Kvist, M., Jozsa, L., Jarvinen, M.J., Kvist, H. Chronic Achilles paratendonitis in athletes: a histological and histochemical study. Pathology 19:1-11, 1987.
11. Schepsis, A. A., Leach, R. E. Surgical management of Achilles tendinitis. Am. J. Sport Med. 15:308-315, 1987.
12. Postacchini, F., DiCastro, A. Subtotal ossification of the Achilles tendon case report. Ital J. Orthop. Traumatol. 4:529-32, 1983.
13. Kleiger, B. The Posterior calcaneal turbicle impingement syndrome. Orthop. Review 5:487-93, 1988.
14. Raynor, K. J., McDonald, R. J., Edelman, R. D., Parkinson, D. E. Ossification of the Achilles tendon. J. Am. Podiatric Med. Assoc. 12:688-90, 1986.
15. Marczak, L., Gelsomino, S., Lusk, D.. Calcified tendo-achilles insertion: a new surgical approach. J. Foot Surg. 5:457-9, 1991.
Surgery for Chronic Achilles Problems : Figure Legends
Figure 1 A & B Abnormal Paratenon shown in MRI (A) and intra-operatively (B).
Figure 2 Mucoid degeneration of Paratenon (in forceps) and focal degeneration of achilles tendon (arrow).
Figure 3A & B MRI showing fusiform, bulbous swelling of Achilles with partial tear (A) and intra-tendonous degeneration (B).
Figure 4 Same patient's achilles as in Figures 3 A &B in the region of chronic inflammation.
Figure 5 Excision of intra-tendonous degeneration (same patient as in Figure 4).
Figure 6 A & B Incision placement for excision of achilles tendocalcinosis and associated Haglunds deformity.
Figure 7A XRAY of achilles tendocalcinosis to be excised.
7B Area of tendocalcinosis to be excised. (Note: the posterior superior aspect of the calcaneus may be resected)
Figures 8 A,B &C Inserted Mitek G II Anchors for achilles tenodesis.
Figure 9 Repair of the achilles tendon after insertion of Mitek G II Anchors.
| PT.No. | AGE/SEX | DIAGNOSIS | PROCEDURE | FOOT TYPE | PRE-OP COMPLICATIONS | RETURN TO DESIRED ATHLETIC ACTIVITY |
| 1 | 27/M | L Paratendonosis | Peritenolysis | FF Varus | None | 3 Wks |
| 2 | 25/M | L Paratendonosis | Peritenolysis | PFFR, 2-5 Varus | None | 5 Wks |
| 3 | 31/M | R Paratendonosis | Peritenolysis & Tendonitis | Neutral & Small Focal | None | 6 Wks |
| 4 | 35/M | B Paratendonosis | Defect Excision Peritenoloysis | FF Varus | None | 3.5 Wks |
| 5 | 39/M | B Tendonosis | Excision of Mucoid Degeneration | FF Varus | None | 12 Wks |
| 6 | 65/M | R Tendonosis & Partial Rupture | Excision of Mucoid Degeneration & Repair of Rupture | RF Varus & Equinus | None | 20 Wks |
| 7 | 59/M | R Tendonosis | Excision of Mucoid Degeneration | Equinus | None | 20 Wks |
| 8 | 31/M | L Tendocalcinosis | Excision of Tendocalcinosis | FF Valgus | None | 12 Wks |
| 9 | 51/M | R Tendocalcinosis | Excision of Tendocalcinosis | FF Valgus | None | 10 Wks |
| 10 | 48/M | L Tendocalcinosis Myositis Ossificans | Excision of Tendocalcinosis | FF Valgus | Reoccurance of Bursitis | 10 Wks |
| 11 | 63/M | R Tendocalcinosis | "/Tenodesis | FF Varus | None | 14 Wks |
| 12 | 34/M | R Tendocalcinosis | "/Tenodesis | FF Varus | Suture Knot Irritation | 12 Wks |
| 13 | 47/M | R Tendocalcinosis | "/Tenodesis | FF Varus / H. Rigidus | None | 12 Wks |
| 14 | 51/M | R Tendocalcinosis | "/Tenodesis | FF Valgus | None | 14 Wks |
| 15 | 70/M | L Tendocalcinosis | "/Tenodesis | FF Valgus | None | 16 Wks |
| 16 | 63/F | R Tendocalcinosis | "/Tenodesis | FF Varus | Superficial Wound Infection | 16 Wks |
| 17 | 66/F | R Tendocalcinosis | "/Tenodesis | FF Varus | None | 14 Wks |
| 18 | 44/F | R Tendocalcinosis | "/Tenodesis | FF Varus | None | 12 Wks |
| 19 | 53/M | L Achilles Avulsion | Tenodesis | FF Varus | None | 24 Wks |
Abbreviations:
R = Right RF = Rearfoot
L = Left FF = Forefoot
B = Bilateral PFFR = Plantarflexed First Ray
Wks = Weeks
Home | About Dr. Saxena | Articles | Appointments | Shoe List | Orthoses
Medial Distal Tibial Syndrome (Shin Splints) | Sever's Disease/Calcaneal Apophysitis
Ankle Sprains & Calf Strains | Injury Prevention | Heel Pain | Achilles Heel | Ankle Stretching, Rehabilitation & Taping
Return to Sports After Injury | Cycling | Marathons | Videos | Recommended Books | Links
Friends & Patients | Legal Notice | Privacy Statement | Site Map
Copyright © Amol Saxena, DPM - Sports Medicine & Surgery of the Foot & Ankle
Web Site Design, Hosting & Maintenance By Catalyst Marketing Innovations, LLC/ Worry Free Websites